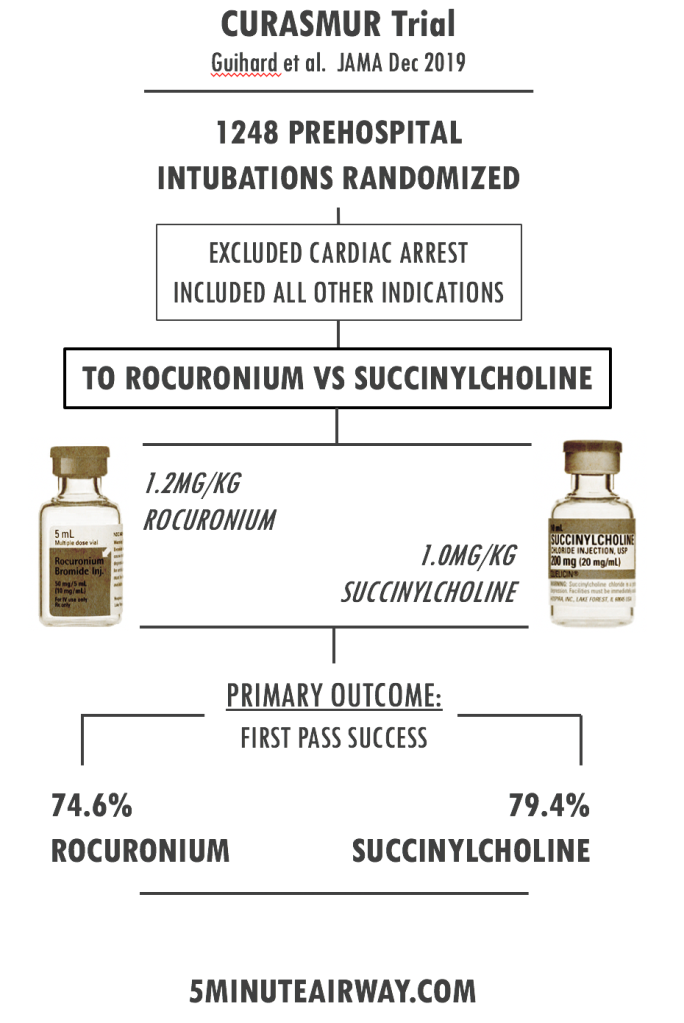
Effect of Rocuronium vs Succinylcholine on Endotracheal Intubation Success Rate Among Patients Undergoing Out-of-Hospital Rapid Sequence Intubation. A Randomized Clinical Trial. JAMA December 2019.
With rising popularity of rocuronium, this publication is a timely addition to debate regarding the ultimate paralytic in RSI. As we’ll see, the debate is definitely not settled and extrapolating this study to general practice may be difficult. Rocuronium was demonstrated to be not non-inferior to succinylcholine. Depending on the camp you’re in, you may find succinylcholine gets one leg up on roc or you’ll identify one of many problems with this study that keeps rocuronium as your paralytic of choice.
METHODS:
- Multicenter trial comparing rocuronium 1.2mg/kg versus succinylcholine 1.0mg/kg in emergent prehospital intubations in the French EMS system.
- 1248 patients ultimately randomized.
- Intubations were performed by either emergency physicians or anesthesiologist with minimum 2 years of experience.
- Inductions meds were either etomidate or ketamine with a strong favor towards etomidate.
- Cardiac arrest patients were excluded.
- Recommended to perform intubation 60 seconds after paralytic was given.
- A non-inferiority margin of 7% was chosen based on prior studies comparing rocuronium to succinylcholine.
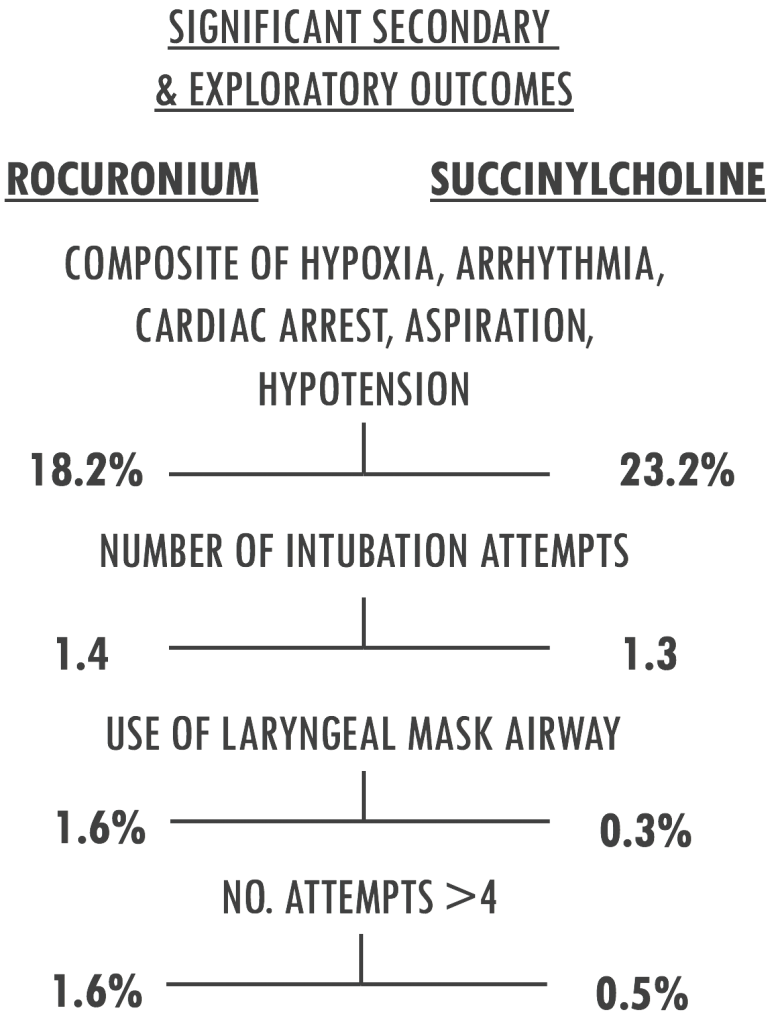
RESULTS:
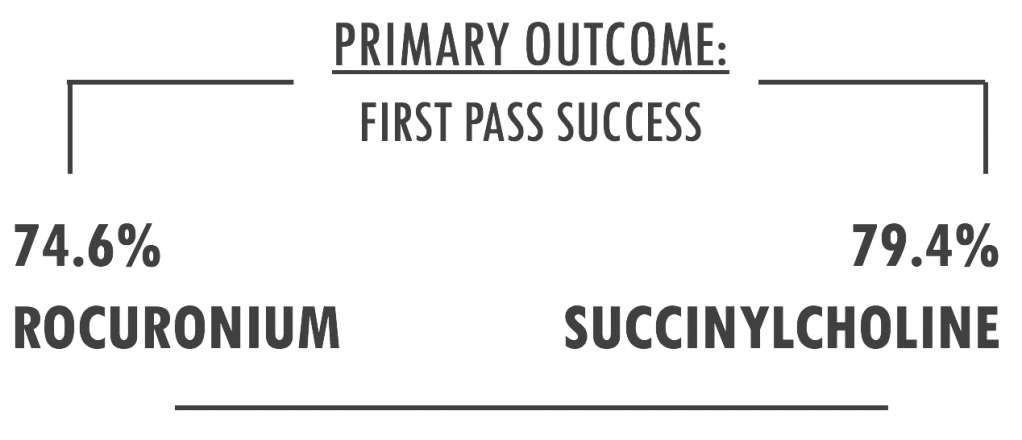
No significant difference in secondary outcomes of Intubation Difficulty Scale score, Copenhagen score, or use of alternative intubation techniques with the exception of LMA.
DISCUSSION:
ONE: What do we already know?
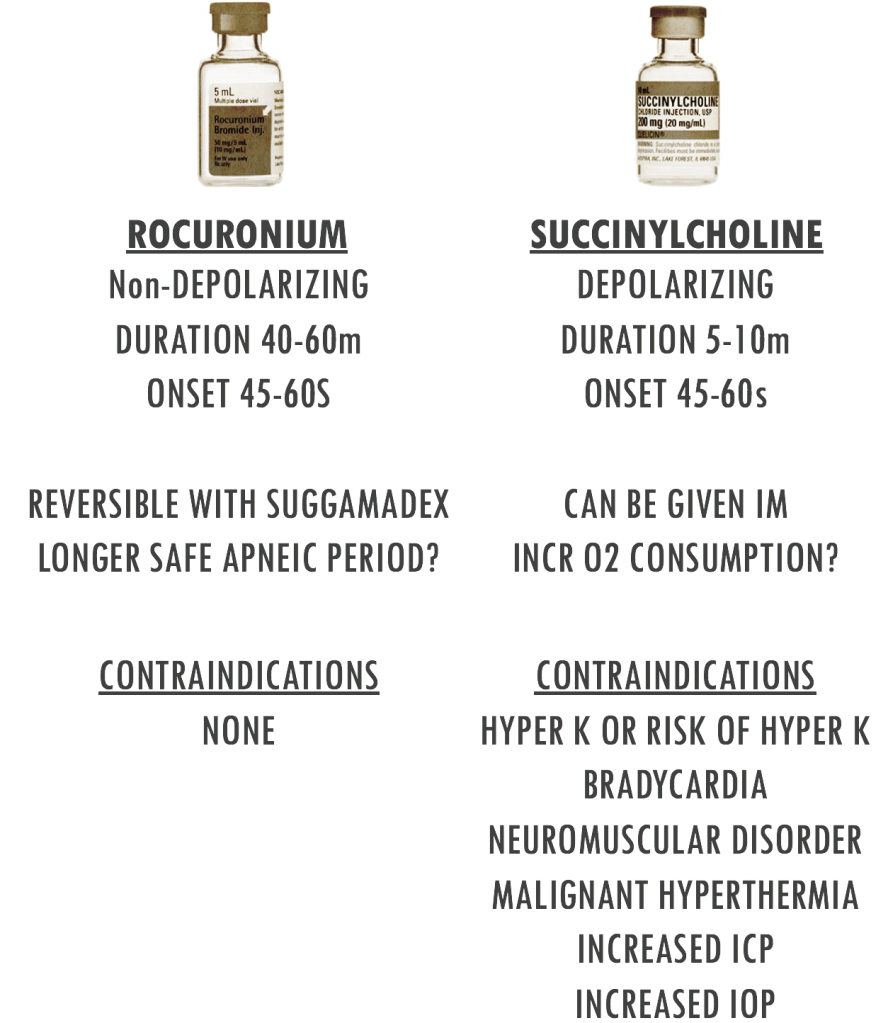
The authors do a good job of pointing out a paucity of prospective, randomized data to explore the debate of which agent facilitates intubation in emergent conditions. Data from the NEAR registry suggests that rocuronium is as good as succinylcholine. Conversely, the most recent Cochrane review would suggest succinylcholine is the preferred agent to provide ideal intubating conditions. This is in addition to a multitude of other studies which are largely OR-based and are neither prospective-randomized trials or in critically ill patients. Without an exhaustive review of ALL the literature, the general difference between the two is:
TWO: Does this study apply to your population?
The French EMS system sounds vastly different from our U.S system. This study utilized pre-hospital physicians for airway management. One of the main fear with succinylcholine is the patient with an unanticipated K of 7.8 meq/L. This may represent real risk if you’re working with an undifferentiated population in the ED. That said, if your clinical context is an ICU, perhaps you’ll be less worried about undiscovered hyperkalemia.
Additionally, the first pass success rates are on the low side, likely reflecting the numerous additional challenges of the pre-hospital arena. Most benchmark studies place first pass success in the mid-to-upper 80’s with recent studies being well into the 90’s. If you’re Hennepin Co. and have a first pass success rate of 98% when using the bougie, its doubtful your paralytic choice is making much of a difference. Consider your clinical context and how this study relates.
THREE: Pragmatic results?
First pass success is a great marker for real-world application and for airway research; it is well known that repeated attempts are associated with adverse outcomes and increased likelihood of catastrophic events such as severe hypoxia and cardiac arrest. But is it a great marker for a paralytic comparison? The answer should be yes. However, the authors recommended intubation occur 60 seconds after meds are pushed. At this time interval, both paralytics likely had full or near full effect, quite possibly negating a true difference between the two. While we don’t know metrics such as duration of intubation attempt, time to first attempt, time to desaturation etc, it is for these reasons many other head to head trials have used time to “ideal intubation conditions” as a primary outcome, although with less pragmatic results.
FOUR: What about the doses?
Props for using higher doses of roc. The question inevitably will be, should they have used even higher doses? Would 1.6mg/kg of roc have shown to be more competitive with the dose of succinylcholine? Data suggesting this dose is actually quite limited despite the popularity. OR would 1.5mg/kg of succinylcholine even demonstrate a greater difference between the two? Studies comparing doses of succinylcholine demonstrate faster results at higher doses but with more muscle myalgia – not necessarily a concern in critical intubations.
FIVE: what the heck is “failed to not meet the non-inferior-inferiority- challenge-hypothesis.”
Or something like that. While 7% was the difference to beat, this number was fairly arbitrary chosen; it was based on prior research in the field which was limited. The authors even state in the limitations, “the noninferiority margin of 7% that was selected was based in part on an expert opinion, which can be considered as a methodological limitation”. Furthermore, this cutoff defines this as a positive or negative study. Had the researchers determined based on expert opinion that 4% was a reasonable difference, the headline would read, “Rocuronium non-inferior to succinylcholine.” Ultimately, no one is going to be stoked with this aspect of the trial but a number had to be chosen and 7% is what they chose.
LAST: Will the debate ever end?
The margins in this study are small and likelihood of one agent ever truly dominating over the other is very low. However, for those entrenched in one camp or the other, this study will likely prove as confirmation of pre-held opinion. Ultimately, in the absence of a contraindication, both agents when dosed appropriately are excellent at achieving rapid, repeatable results.
Written by Terren Trott (@tsquaredmd) and peer-reviewed by Chris Belcher (@seebelcher236)
See Also:
- EM Nerd: Case of Adjacent Contradictions. Rory Spiegel. Dec 2019.
- RSI Meds in Obesity
References
- Rocuronium vs. succinylcholine for rapid sequence intubation: a Cochrane systematic review. Tran DTT.. Anesthesia 2017
- Emergency Department Intubation Success With Succinylcholine Versus Rocuronium: A National Emergency Airway Registry Study. April MD.. Ann Emerg Med. 2018
- Desaturation following rapid sequence induction using succinylcholine vs. rocuronium in overweight patients. Tang L. Acta Anaesthesiol Scand. 2011